Early identification of sepsis is critical for patient survival, yet it remains a significant challenge[1]. Nurses play a vital role in this process by routinely monitoring patients for signs of sepsis. This article highlights key aspects of identification and management for healthcare professionals,
Identifying Sepsis – The Tools
- Systemic Inflammatory Response Syndrome (SIRS): Any patient presenting with two or more SIRS and a suspected infective source is deemed to have sepsis. Further evaluation for organ dysfunction (severe sepsis) and mortality risk is necessary.
- National Early Warning Score (NEWS2): This tool, developed by the Royal College of Physicians, is useful for identifying unwell patients and performs well in those with suspected sepsis or time-dependant infection. A score of 5 or more warrants sepsis screening.[2]
- Children: Children often do not have overt symptoms, and compensate well during a disease process like sepsis, with subtle changes which can be easily missed. Early escalation to senior support is therefore crucial. In addition, the use of a Paediatric Early Warning Score (PEWS) with a defined escalation plan is recommended.
It’s estimated that there are around 123,000 cases of sepsis each year in England, with around 1,000 of these cases reported in children under five1
“Education and training is the golden thread in improving recognition, treatment and positive outcomes of sepsis in children. We are working with Health Education England to make sure all health professionals have the knowledge and skills to identify and treat sepsis.” NHS England.[3]
Management Strategies
The majority of clinical evidence on sepsis is focused on severe sepsis and septic shock – there is little on uncomplicated sepsis. Despite this, in all cases of sepsis, patients need immediate intervention to determine severity and prevent further deterioration.
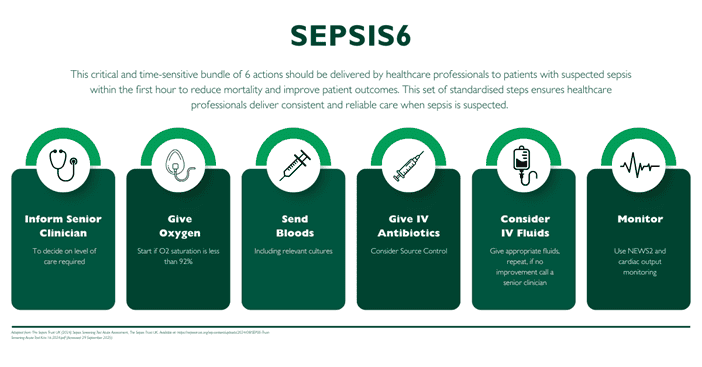
Sepsis Six Care Bundle[4]
Developed by the UK Sepsis Trust, this critical and time-sensitive bundle of 6 actions should be delivered by healthcare professionals to patients with suspected sepsis within the first hour to reduce mortality and improve patient outcomes.
This set of standardised steps ensures healthcare professionals deliver consistent and reliable care when sepsis is suspected. The steps include oxygen administration, blood cultures, antibiotic initiation, fluid resuscitation, lactate measurement, and monitoring urine output.
Within the first hour, you must:
- Inform Senior Clinician
- Give Oxygen, if required
- Send bloods, including relevant cultures
- Consider IV Antibiotics, think source control
- Consider IV Fluids
- Continued Monitoring
Detailed Look at Fluid Therapy (Step Five of Sepsis Six):
Looking more closely at step five, fluid resuscitation, which is crucial for improving tissue oxygen delivery in sepsis cases. Cardiac output is a key factor in calculating oxygen delivery and therefore determining the effectiveness of fluid therapy.
- Cardiac Output: This value reflects the amount of blood pumped by the heart per minute. It is calculated by multiplying stroke volume (amount of blood ejected per heartbeat) by heart rate.
The body will naturally increase the heart rate to attempt to overcome a low blood pressure or vasodilatation. This effect is frequently seen early in sepsis.
The stroke volume is dependent on two variables:
- Preload: the volume of blood in the heart/ circulating volume.
A hypovolaemic patient will have a low preload and therefore a low stroke volume - Afterload: the pressure that the ventricle must overcome to eject blood/ the ‘systemic vascular resistance’
In sepsis, the afterload is usually low, and the heart rate and contractility will need to increase to maintain blood pressure. In early stages of sepsis, the circulation is described as hyperdynamic: cardiac output initially rises.
Sepsis causes complex dysfunction in the body’s inflammatory and coagulopathy pathways, leading to vasodilatation, vessel leakage and increased metabolic demands. This effect increases oxygen demand which, combined with intravascular losses, causes hypoperfusion and ischaemia at cellular levels[5] Porth, MC.
The aims of fluid therapy are:
- To correct absolute and relative hypovolaemia
- To bring the patient’s pulse, blood pressure, mental state, lactate and urine output within target
- To do this judiciously, and to avoid pushing the patient into overload.
Fluid Overload
In sepsis, timely fluid resuscitation is crucial to improve tissue perfusion and oxygen delivery. However, excessive fluids can have the opposite effect:
- Worsened tissue perfusion – Too much fluid in the bloodstream can reduce blood flow to vital organs.
- Increased mortality risk – Fluid overload can exacerbate complications and raise the risk of death in sepsis patients.
Therefore, careful monitoring and personalised fluid management are essential in sepsis treatment. Clinicians need to balance the need for adequate fluid resuscitation with the risk of fluid overload.
Read more about Avoiding Fluid Overload: https://campusvygon.com/uk/articles/fluid-therapy-navigating-the-delicate-balance-and-avoiding-overload/
Using Cardiac Output Monitors to Manage and Treat Sepsis
A cardiac output monitor will provide in-depth information on the patient’s status, specifically regarding the individual elements of stroke volume. This will give you a much better understanding of your patient’s condition and when to give fluids, and how much, therefore reducing the risk of fluid overload for the patient.
Sepsis is a dynamic condition, that can improve as quickly as it can worsen so it is important to use monitoring systems that provide real-time continuous monitoring as well as trend data so you can see immediate and long-term changes in your patient and their condition.
When a Cardiac Output Monitor Is Not Available
Most people will present for the first time with sepsis in environments where a cardiac output monitor may not be available, or the treating healthcare professional may not be able to access the patient’s blood flow for any reason. This may be in environments such as within primary care, in the Emergency Department or Medical/Surgical Admissions Unit or as a deteriorating patient on the ward, not in Intensive Care.
As blood flow (cardiac output) falls, urine output also declines, therefore it is important to closely observe urine output as an indicator of declining blood flow, as it may serve as an early indicator of sepsis. This monitoring is essential for guiding further fluid challenges and can help to identify a problem with circulatory compromise before a drop blood pressure occurs.
It is important to use all clinical observations at your disposal, especially where a cardiac output monitor is not available to your patient, for example, monitoring factors such as the skin, respiratory and metabolism, which could all also give insights into your patient’s condition.
Conclusion
Sepsis is a complex and time-sensitive condition. Early identification and implementation of the Sepsis Six Care Bundle is crucial for improving patient outcomes. Healthcare professionals play a vital role in recognising the signs of sepsis and initiating appropriate management strategies.
- Stay vigilant for signs and symptoms of sepsis in your patients.
- Utilise tools like NEWS22 and PEWS for early identification.
- Implement the Sepsis Six Care Bundle promptly for suspected cases.
- Advocate for ongoing education and training on sepsis management.
Remember, early recognition and intervention are key to saving lives in sepsis.
[1] Slade E et al (2003) The Surviving Sepsis Campaign: raising awareness to reduce mortality. Critical Care; 7, 1-2.
[2] Royal College of Physicians (2012) National Early Warning Score (NEWS): Standardising the Assessment of Acute-illness Severity in the NHS.
[3] NHS England. New learning package designed to help clinicians spot the early sign of sepsis in children and infants. [Online]. Available from: https://www.hee.nhs.uk/news-blogs-events/news/new-learning-package-designed-help-clinicians-spot-early-sign-sepsis-children-infants [Accessed 31 July 2024].
[4] The Sepsis Trust UK (2024) Sepsis Screening Tool Acute Assessment, The Sepsis Trust UK. Available at: https://sepsistrust.org/wp-content/uploads/2024/08/SEPSIS-Trust-Screening-Acute-Tool-Kits-16-2024.pdf (Accessed: 29 September 2025).
[5] Porth MC (2005) Pathophysiology: Concepts of Altered Health States. Philadelphia PA: Lippincott Williams & Wilkins.



