Healthcare faces mounting challenges from climate change and rising operational costs. A significant portion of its carbon footprint stems from plastic waste, and the energy demands of departments such as operating theatres and intensive care units. To mitigate this, it is vital to adopt clinical practices that deliver both environmental and economic benefits without compromising patient care.
In addition, the European Society of Anesthesiology and Intensive Care (ESAIC), the World Federation of Societies of Anesthesiologists (WFSA), and the European Society of Intensive Care Medicine (ESICM) recently called for action to promote and favour green solutions in anaesthesia and critical care.[1], [2], [3].
This article explores a recent study in Critical Care Science, where Michard et al. (2025) propose green pulse wave analysis (PWA) as a sustainable and cost-effective alternative to traditional perioperative haemodynamic monitoring, which is particularly valuable for middle-income countries, with broader relevance across healthcare systems[4].
The environmental and human impact of cardiac output monitoring
Healthcare systems worldwide grapple with the dual pressures of climate change and escalating operational costs1,2. With a carbon footprint so significant, the global healthcare sector, if considered a country would rank among the top ten carbon emitters. This significant carbon footprint is dominated by large volumes of plastic waste2,[5] and the substantial energy used for heating, ventilation, and air conditioning[6], especially in departments such as operating theatres and intensive care units which particularly resource intensive.
According to the study by Michard et al, it is therefore important to rethink perioperative haemodynamic monitoring, considering alternatives to traditional healthcare methods which have a proven positive impact on both patient care and the financial and environmental factors4.
The Environmental Impact
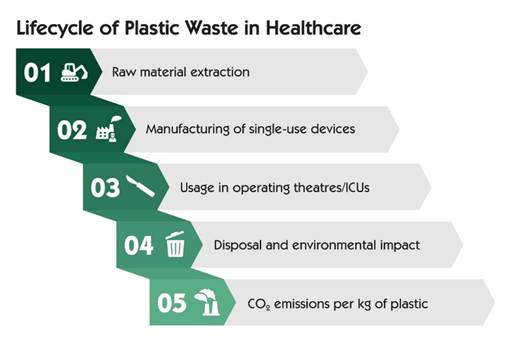
While the broader environmental footprint of healthcare is well recognised, the specific impact of perioperative monitoring deserves closer attention. Operating theatres and ICUs not only consume large amounts of energy for climate control, but also generate considerable plastic waste through single-use devices and packaging.
The study by Michard et al. draws attention to the full lifecycle emissions of these materials from raw material extraction to waste disposal4. It is also important to note that for each kilogram of plastic contributes to approximately three kilograms of CO₂[7]. This helps to reinforce the need to reassess traditional haemodynamic monitoring methods, not only for their clinical value, but also for their environmental and economic consequences.
The Human Impact
Beyond its environmental toll, plastic waste is increasingly recognised as a potential health hazard. Micro- and nano-plastics have now been detected in human organs, raising concerns about their long-term impact. While the full extent of their health effects remain unknown, emerging evidence suggests a troubling link to increased risks to cardiovascular health[8].
A study found micro- and nano-plastics present in 60% of atheroma cases, with an association between their presence and a significant increase in cardiovascular adverse events[9]. These findings highlight the urgent need to reduce plastic use in clinical environments, not only to cut emissions, but to address emerging health risks linked to microplastic exposure.
Rethinking Cardiac Output Monitoring
Despite strong clinical interest in perioperative cardiac output monitoring, its adoption remains limited, particularly in high-risk surgical patients due to the cost and availability of equipment[10]. This highlights a critical barrier: traditional haemodynamic monitoring systems are often expensive, brand-specific, and reliant on single-use components, making them both financially and environmentally unsustainable.
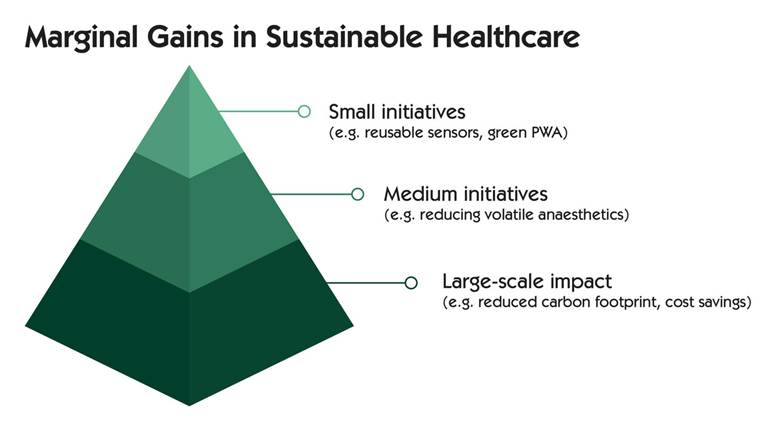
In response, Michard et al. propose a shift towards more sustainable practices. Several strategies have been suggested to reduce the carbon footprint of anaesthesia and critical care, including the use of reusable laryngoscope blades and pulse oximetry sensors, which align with circular economy principles. Reducing the use of volatile anaesthetics (potent greenhouse gases) is another important step5.
When advanced monitoring is clinically justified, such as in cases of severe pulmonary hypertension or pulmonary oedema, techniques like pulmonary artery pressure monitoring or transpulmonary thermodilution may still be appropriate. However, for routine perioperative care, less resource-intensive alternatives are available.
Uncalibrated pulse wave analysis (PWA) techniques are increasingly used across Europe, with 92% of anaesthesiologists reporting their use during surgery10. These methods support fluid management and have been shown to reduce postoperative complications[11]. Importantly, not all PWA systems are created equal. Some require dedicated pressure transducers, which are larger, more plastic-intensive devices with rigid packaging, while others operate with standard transducers which are more commonly found in clinical settings[12].
The latter category, now referred to as “green cardiac output monitoring”, offers a practical and environmentally conscious alternative. These systems reduce plastic waste, lower costs, and maintain clinical accuracy, making them a compelling choice for departments seeking to align patient care with sustainability goals12, [13].
The Benefits of the Solution:
Before green PWA techniques can be widely adopted in perioperative cardiac output monitoring, two factors must be considered: clinical reliability and cost. Encouragingly, comparative studies suggest that these systems perform better than traditional PWA methods with higher accuracy, precision and in tracking cardiac output changes.
Romagnoli et al. found that MostCareUp (Vygon, France) had a two-to-three times lower percentage error rate than FloTrac[14]. Hadian et al. reported narrower limits of agreement and reduced bias with LiDCOrapid[15] (Masimo, USA), while Mukkamala et al. observed a substantially lower bias with Argos (Retia, USA) compared to FloTrac[16]. All three systems operate with standard pressure transducers, classifying them as green PWA technologies12,13.
Current evidence suggests that adopting green PWA does not compromise accuracy or precision. However, further studies comparing green and non-green PWA techniques, would help confirm their performance across broader clinical contexts.
In terms of cost, green PWA systems offer significant savings. A nationwide French study estimated annual savings of €67 million through their use, which is equivalent to the salaries of over 2,000 French nurses or the purchase of more than 10,000 handheld ultrasound devices13.
Conclusion
Green pulse wave analysis (PWA) presents a clinically reliable, cost-effective and environmentally conscious alternative for perioperative cardiac output monitoring. Uncalibrated PWA techniques are already widely used by anaesthetists, and studies show that green systems, those using standard pressure transducers, perform as well as those requiring dedicated components. This makes them a practical and scalable solution for improving patient care while supporting sustainability goals across healthcare systems.
By minimising plastic waste and associated CO₂ emissions, green PWA can reduce hospital costs and improve access to advanced monitoring, especially in resource-limited settings. This shift supports both clinical excellence and environmental responsibility, making it a valuable step towards more sustainable healthcare.
While a single green initiative may only modestly affect a hospital’s carbon footprint, the cumulative effect of multiple marginal gains can lead to significant sustainability improvements.
References
[1] White SM, Shelton CL, Gelb AW, Lawson C, McGain F, Muret J, et al.; representing the World Federation of Societies of Anaesthesiologists Global Working Group on Environmental Sustainability in Anaesthesia. Principles of environmentally-sustainable anaesthesia: a global consensus statement from the World Federation of Societies of Anaesthesiologists. Anaesthesia. 2022;77(2):201-12
[2] Buhre W, De Robertis E, Gonzalez-Pizarro P. The Glasgow declaration on sustainability in anaesthesiology and intensive care. Eur J Anaesthesiol. 2023;40(7):461-4
[3] De Waele JJ, Hunfeld N, Baid H, Ferrer R, Iliopoulou K, Ioan AM, et al. Environmental sustainability in intensive care: the path forward. An ESICM green paper. Intensive Care Med. 2024; 50(11):1729-39
[4] Michard F. Going green for perioperative hemodynamic monitoring: a golden opportunity for middle-income countries [Internet]. Biasi Cavalcanti A, editor. Critical Care Science. Online: Critical Care Science; 2025 Jan [cited 2025 Oct 24]. Available from: https://criticalcarescience.org/wp-content/uploads/sites/7/articles_xml/2965-2774-ccsci-37-e20250379/2965-2774-ccsci-37-e20250379.pdf
[5] McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br J Anaesth. 2020;125(5):680-92
[6] McGain F, Burnham JP, Lau R, Aye L, Kollef MH, McAlister S. The carbon footprint of treating patients with septic shock in the intensive care unit. Crit Care Resusc. 2018;20(4):304-12
[7] McGain F, Sheridan N, Wickramarachchi K, Yates S, Chan B, McAlister S. Carbon footprint of general, regional, and combined anesthesia for total knee replacements. Anesthesiology. 2021;135(6):976-91.
[8] Thompson RC, Courtene-Jones W, Boucher J, Pahl S, Raubenheimer K, Koelmans AA. Twenty years of microplastic pollution research-what have we learned? Science. 2024;386(6720):eadl2746
[9] Marfella R, Prattichizzo F, Sardu C, Fulgenzi G, Graciotti L, Spadoni T, et al. Microplastics and nanoplastics in atheromas and cardiovascular events. N Engl J Med. 2024;390(10):900-10.
[10] Flick M, Joosten A, Scheeren TW, Duranteau J, Saugel B. Haemodynamic monitoring and management in patients having noncardiac surgery: a survey among members of the European Society of Anaesthesia and Intensive Care. Eur J Anaesthesiol Intensive Care. 2023;2(1):e0017.
[11] Michard F, Giglio MT, Brienza N. Perioperative goal-directed therapy with uncalibrated pulse contour methods: impact on fluid management and postoperative outcome. Br J Anaesth. 2017;119(1):22-30.
[12] Michard F, Romagnoli S, Saugel B. Make my haemodynamic monitor GREEN: sustainable monitoring solutions. Br J Anaesth. 2024;133(6):1367-70
[13] Michard F, Futier E, Desebbe O, Biais M, Guinot PG, Leone M, et al. Pulse contour techniques for perioperative hemodynamic monitoring: a nationwide carbon footprint and cost estimation. Anaesth Crit Care Pain Med. 2023;42(5):101239.
[14] Romagnoli S, Ricci Z, Romano SM, Dimizio F, Bonicolini E, Quattrone D, et al. FloTrac/Vigileo(TM) (third generation) and MostCare(®)/PRAM versus echocardiography for cardiac output estimation in vascular surgery. J Cardiothorac Vasc Anesth. 2013;27(6):1114-21.
[15] Hadian M, Kim HK, Severyn DA, Pinsky MR. Cross-comparison of cardiac output trending accuracy of LiDCO, PiCCO, FloTrac and pulmonary artery catheters. Crit Care. 2010;14(6):R212
[16] Mukkamala R, Kohl BA, Mahajan A. Comparison of accuracy of two uncalibrated pulse contour cardiac output monitors in off-pump coronary artery bypass surgery patients using pulmonary artery catheter-thermodilution as a reference. BMC Anesthesiol. 2021;21(1):189.