The VAD (vascular access device) insertion experience varies between patients. For individuals with difficult intravenous access (DIVA), the process can become traumatic and notably painful. According to Blanco (2019), DIVA affects up to one-third of critically ill patients.
Ensuring the utmost comfort and well-being for these patients should be a primary concern for healthcare practitioners. This necessitates a clear definition of DIVA as well as proper guidelines for their care.
WHAT IS A DIVA PATIENT?
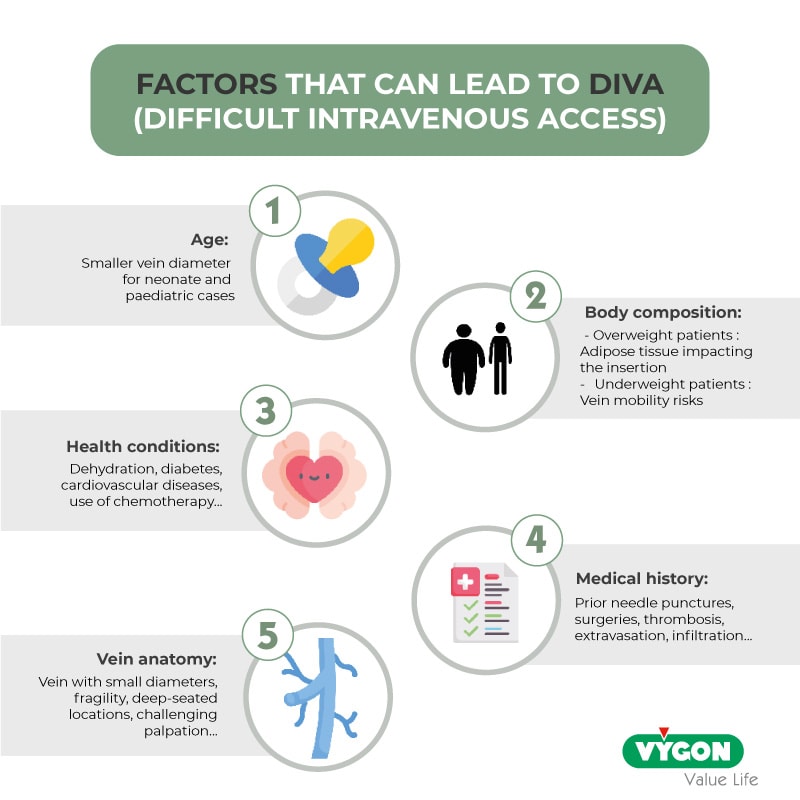
According to Sou Y et al. (2017), DIVA refers to instances where catheter placement into a vein isn’t achieved in a single attempt. These challenges can stem from various factors:
The VAD insertion experience of DIVA patients
Invisible and non-palpable veins often result in numerous punctures and attempts for VAD insertion, causing discomfort and pain for patients.
Additionally, the challenge of accessing veins can result in treatment delays, prolonging the procedure beyond typical timelines and intensifying the apprehension experienced by DIVA patients.
Furthermore, the psychological impact of repeated painful cannulations should not be overlooked. They can lead to distress, instil anxiety, and make the procedure a significant burden for the patient.
Secure and comfortable care for DIVA patients
The various factors affecting catheter insertion success necessitate a tailored approach for optimal patient care:
Identification of potential DIVA patients
Recognizing DIVA patients enables the adoption of a personalized and efficient approach. Accordingly, evaluating the patient’s age, body type, and health conditions becomes essential. Additionally, reviewing the patient’s medical history allows practitioners to anticipate challenges that might arise during VAD insertion.
Vein grading scales
Prioritizing the identification of the optimal vein for catheter insertion is essential with DIVA patients. Vein grading scales have been developed to streamline this process.
The modified A-DIVA scale offers a structured approach to identifying patients with challenging intravenous access. This scale evaluates factors like prior difficulties with intravenous cannulation, practitioners’ anticipation of challenges, palpability and visibility of the target vein, and vein diameter (up to 2 millimetres). Subsequently, the scores are categorized into low, moderate, and high-risk groups. The latter indicates a higher risk of encountering difficulties during intravenous access.
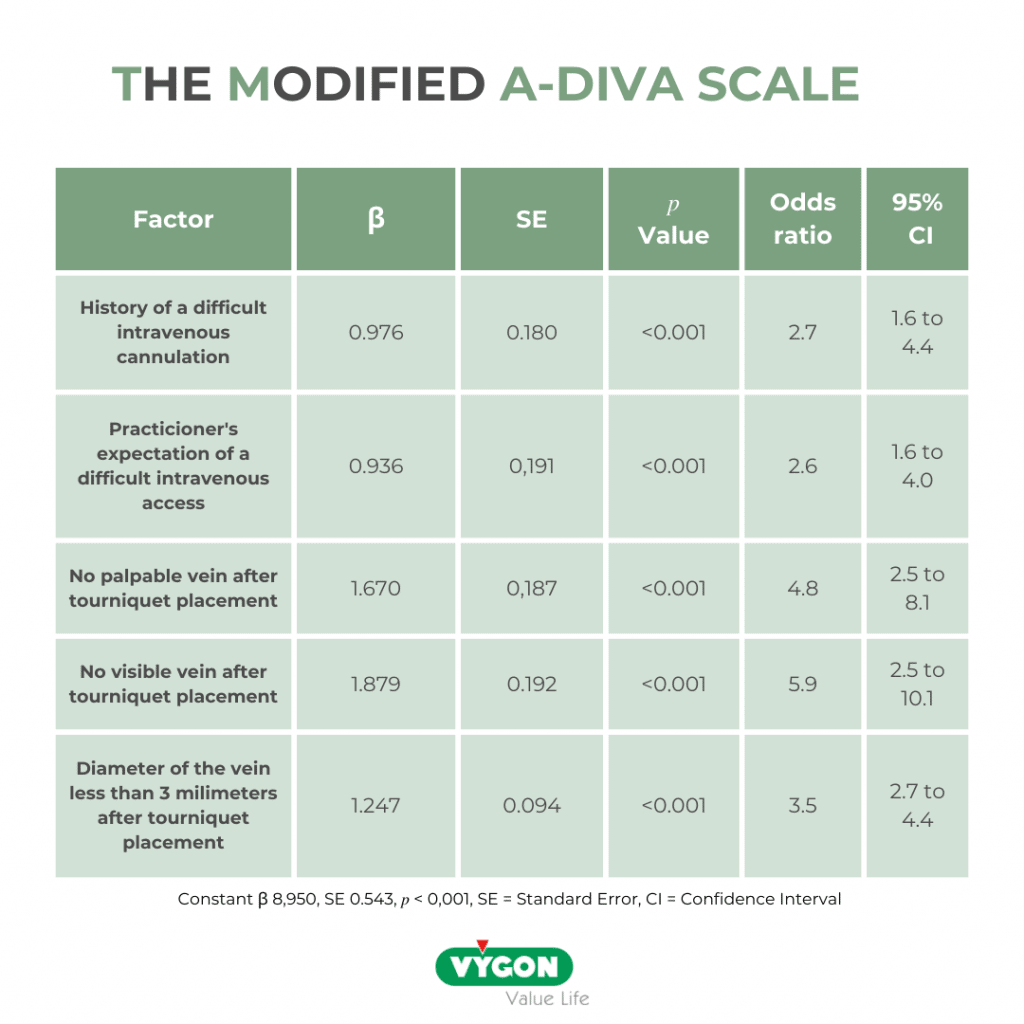
Image: The Modified A-Diva Scale as a predictive tool for prospective identification of adult patients and risk of a difficult intravenous access (Van Loon et al. 2019)
Vein visualisation technologies
Vein visualisation technologies employ various imaging techniques that allow better visibility for the veins, effectively reducing the number of cannulation attempts.
Literature strongly advocates for the utilization of ultrasound in the case of DIVA patients. By providing imaging of veins beneath the skin’s surface, it significantly enhances the precision and accuracy of visualizing the vascular anatomy, thus reducing insertion attempts. To illustrate this point, a study led by Vanno Sou et al. (2017) demonstrated a 90% success rate in initial catheter insertion attempts, coupled with marked reductions in pain scores attributed to the use of ultrasound-guided insertion techniques.
Furthermore, alternative techniques like Near-Infrared Imaging (NIR), have proven valuable in locating veins for cannulation. This method involves illuminating the skin using near-infrared light, which is subsequently absorbed by the blood and reflected by nearby tissues. The device’s camera captures this reflection, facilitating enhanced vein visualization.
Topical or local anaesthesia
Topical and local anaesthesia offer valuable benefits for DIVA patients by reducing pain and discomfort during repeated cannulation attempts. Research indicates successful pain management through local anaesthesia application during VAD placement. This approach not only reduces pain but can also ease patient anxiety.
Distraction therapies
The use of distraction therapies can be an effective way of reducing the patient’s anxiety by making them focus on other tasks.
For instance, Digital Sedation has witnessed a notable surge across various medical fields. It can now be an alternate approach to premedication and anti-anxiety medications and has proven to be efficient. By steering patients’ focus toward a virtual reality realm accessed through a headset, Digital Sedation effectively shifts attention from the procedure.
Beyond augmented reality, other relaxation tools and methods can assist in alleviating anxiety. Techniques such as hypnosis, music, games, breathing and mindfulness exercises, or simply interacting with the patient, can guide attention away from the procedure, granting patients greater comfort and ease.
Education and training
Continuous learning and team training can allow a better understanding of DIVA patients as well as the adoption of new reflexes and practices. This proactive approach aims to reduce discomfort and pain associated with multiple cannulations, promoting more patient-centred care.
Prioritizing the safety and comfort of DIVA patients through an individualized approach is crucial. This emphasis on personalized care not only enhances overall well-being but also cultivates a more patient-centred experience. Overall, clear communication with the patient and their involvement throughout the decision-making process can help reduce anxiety and distress.
Bibliography:
- Vanno Sou, Craig McManus, Nicholas Mifflin, Steven A Frost, Julie Ale, Evan Alexandrou. A clinical pathway for the management of difficult venous access. BMC Nursing, 2017. https://pubmed.ncbi.nlm.nih.gov/29176933/
- Hamdan Eren. Difficult Intravenous Access and Its Management. From the edited volume “Ultimate Guide to Outpatient Care”. 2021. https://www.intechopen.com/chapters/75477
- Stagg P L (April 04, 2023) The Adult Difficult Intravenous Access (DIVA) Cognitive Aid: An Evidence-Based Cognitive Aid Prototype for Difficult Peripheral Venous Access. Cureus 15(4): e37135. doi:10.7759/cureus.37135
- Mary Bond, Louise Crathorne, Jaime Peters, Helen Coelho, Marcela Haasova, Chris Cooper, Quentin Milner, Vicki Shawyer, Christopher Hyde & Roy Powell. First do no harm: pain relief for the peripheral venous cannulation of adults, a systematic review and network meta-analysis. BMC Anesthesiology. 2016. https://bmcanesthesiol.biomedcentral.com/articles/10.1186/s12871-016-0252-8
- Rosay H, Laurent C, Delhomme I, Hamon G, Thiot A, Dupre A; Autohypnosis and Virtual Reality decrease preoperative anxiety ASA 2017
- Roberto Kasuo Miyake, Herbert David Zeman, Flavio Henrique Duarte, Rodrigo Kikuchi, Eduardo Ramacciotti, Gunnar Lovhoiden, Carlos Vrancken. Vein imaging: a new method of near infrared imaging, where a processed image is projected onto the skin for the enhancement of vein treatment. Dermatologic Surgery. 2006. https://pubmed.ncbi.nlm.nih.gov/16918565/
- Pablo Blanco. Ultrasound-guided peripheral venous cannulation in critically ill patients: a practical guideline. The Ultrasound Journal. 2019. https://theultrasoundjournal.springeropen.com/articles/10.1186/s13089-019-0144-5



