Pulmonary surfactants along with other therapeutic measures are the treatment of choice for various respiratory conditions. A surfactant deficiency in preterm infants leads to respiratory distress syndrome characterized by poor lung expansion, inadequate gas exchange and atelectasis.
Premature newborns receiving surfactant administration require careful and dedicated nursing care. Great results are found in the small details.
What is pulmonary surfactant?
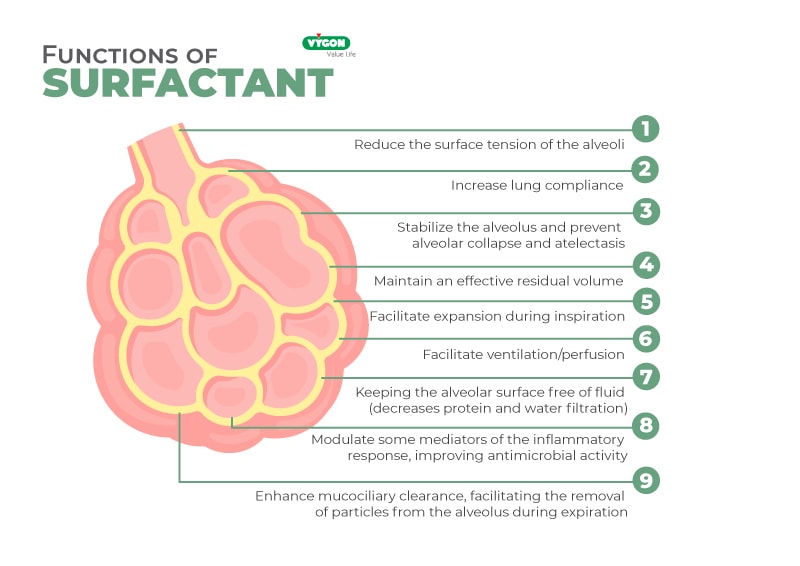
Pulmonary surfactant is a surfactant substance produced by type II pneumocytes, whose concentration in the premature/immature newborn is decreased, leading to the production of respiratory distress syndrome. Surfactant consists of 80% phospholipids, 8% neutral lipids and 12% proteins.
Surfactant production begins at approximately 26 weeks of pregnancy. Its main function is to prevent alveolar collapse and atelectasis. However, prenatally, there are situations that accelerate or delay the appearance of surfactant.
Patients with a shortage of surfactant at birth are usually administered a modified natural extract derived from form porcine or bovine lung or a synthesized solution. Its function is to compensate for this deficit and restore alveolar surface tension. This reduces mortality and air leaks associated with respiratory distress syndrome (RDS).
The administration of corticosteroids increases pulmonary maturity in cases of risk of premature delivery, or when it is necessary to perform a cesarean section as early as possible. Treatment of preterm infants with RDS includes administration of surfactant into the tracheobronchial tree. It is important to note that infants should not be intubated solely for prophylactic surfactant administration.
Types of surfactant
Natural/artificial surfactants administered in the NICU have evolved with the advancement and development of neonatal care. They can be classified into three types:
- First generation of surfactants: protein-free synthetics. The first generation of synthetic surfactants contained dipalmitoyl-phosphatidyl-choline (DPPC), but no proteins. The best known was colfosceril palmitate.
- Second generation of surfactants: natural surfactants of animal origin. The best-known surfactants are those obtained from bovine or pig lungs or from animal lung lavage subjected to chloroform-methanol extraction. The best-known surfactants are derived from bovine, porcine or modified bovine extracts.
- Third generation of surfactants: synthetic surfactants with synthetic peptides or recombinant proteins. Indicated as an agent to decrease surface tension plus other aggregates that increase adsorption.
It is advisable to start treatment as soon as possible after diagnosis. The recommended doses for this type of patient are 200 mg/kg/dose (2.5 ml/kg/dose), which can be administered as a single dose or divided into 2 doses of 100 mg/kg, the first of which should be administered immediately and the second after about 12 hours. If clinical conditions continue to be critical (a/A PO2 ratio <0.22), an additional dose of 100 mg/kg may be administered after an interval of approximately 12 hours.
How to administer surfactant?
What has changed the most in recent years are the different strategies used for surfactant administration combined with different ventilatory modalities and noninvasive methods of ventilation.
One option to administer surfactant and avoid CMV is the intubate-surfactant-extubate (INSURE) technique. With this technique, after intubation, surfactant is administered and then extubated, followed by noninvasive ventilation (NIV).
With the aim of administering exogenous surfactant avoiding CMV, the techniques known as MIST (Minimal Invasive Surfactant Therapy) have emerged. These include nasopharyngeal instillation, administration by laryngeal mask, aerosolization and techniques requiring tracheal catheterization. Among these, the most widely used today is tracheal catheterization, due to its easy applicability, the possibility of administering the surfactant quickly and its effective distribution.
Among the tracheal catheterization techniques, we must highlight the LISA method. This technique uses a thin catheter for the administration of surfactant which is placed through the vocal cords enabling neonates to maintain glottis function and continue spontaneous breathing.
It is important to emphasize that MIST techniques are part of a comprehensive non-invasive approach that supports the concept of a gradual transition to the extrauterine world.
There is also surfactant administration through the technique known as the Cologne method, which consists of introducing a 4-5 FG nasogastric tube (NGT) into the trachea with the aid of Magill forceps, or the Hobart method, developed to dispense with Magill forceps by using an angiocatheter.
The role of nursing in surfactant therapy
Although the administration procedure is traditionally carried out by doctors, nursing professionals play a key role in surfactant therapy as they will be involved during and after the delivery process.
Nursing care during surfactant administration
- Prepare the necessary elements to administer surfactant.
- Participate in the technique sterile or under laminar flow.
- Assess hemodynamic and oxygenation conditions of the newborn.
- Ensure the comfort of the newborn; if possible place the newborn in prone position. This position improves alveolar recruitment.
- Perform radiographic and blood gas monitoring to assess improvement and extubate if appropriate.
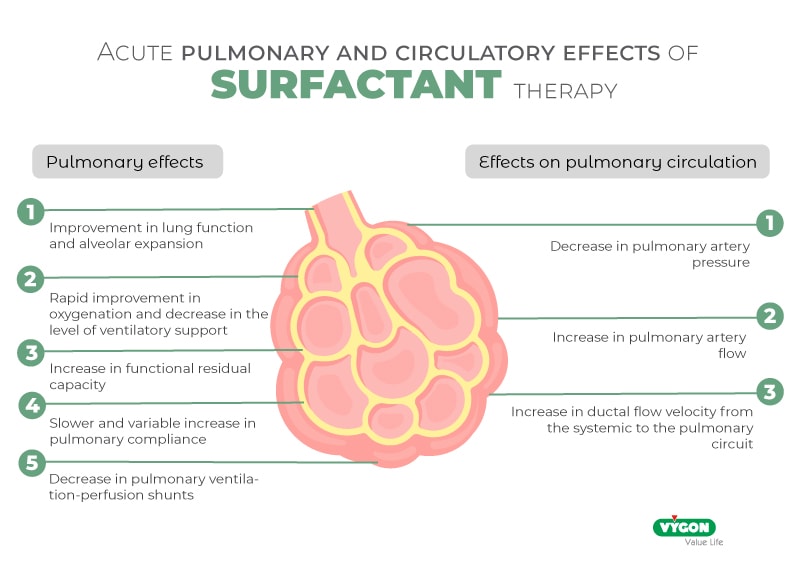
- Actively look for complications of surfactant administration such as pulmonary hemorrhage and ductal opening.
- Do not aspirate the endotracheal tube if possible for up to 6 hours after administration.
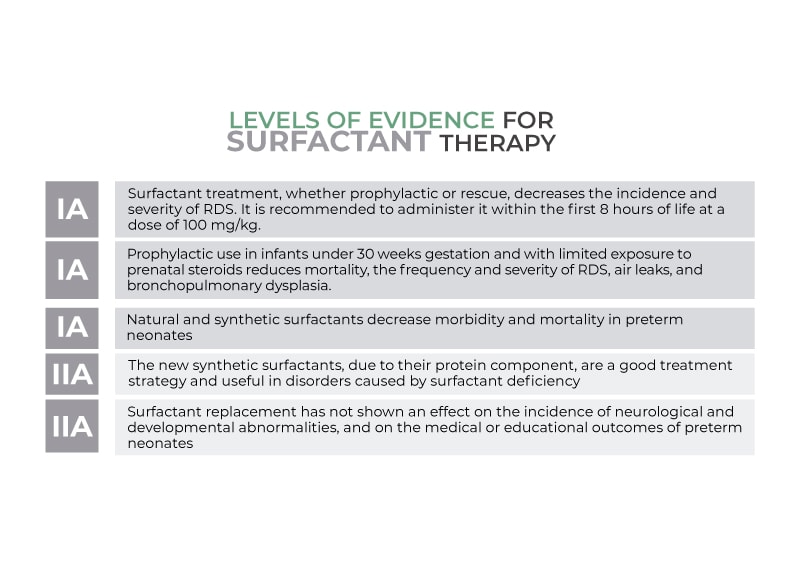
Levels of evidence Ia
- Prophylactic or rescue surfactant treatment decreases the incidence and severity of RDS, recommended to be administered in the first 8hrs of life 100mg/kg.
- Prophylactic use in children under 30 weeks and with little prenatal steroid exposure decreases mortality, frequency and severity of RDS, air leak and BPD.
- Natural and synthetic surfactants decrease morbidity and mortality in preterm infants.
Levels of evidence IIa
- The new synthetic surfactants, because of their protein component, are a good treatment strategy and useful in surfactant deficiency disorders.
- Surfactant replacement has shown no effect on the incidence of neurological and developmental disorders and on medical or educational outcomes in preterm infants.
Bibliography
- Spanish Association of Pediatrics (AEPED). (n.d.). Porcine Pulmonary Surfactant. Pediamecum. Retrieved from https://www.aeped.es/comite-medicamentos/pediamecum/surfactante-pulmonar-porcino
- Batista-Cardenas, N., González-Martínez, M., Menéndez-Sainz, C., & Colomé-Gallegos, E. (2012). Natural Pulmonary Surfactant. Revista Habanera de Ciencias Médicas, 11(1), 78-85. Retrieved from http://www.revhabanera.sld.cu/index.php/rhab/article/view/4362
- Flores-Pérez, J., Rodríguez-Mendoza, L., Álvarez-Delgado, E., Aguilar-Ávila, D., & Cuevas-García, A. (2010). Pulmonary Surfactant: Treatment for Hyaline Membrane Disease. Revista de Especialidades Médico-Quirúrgicas, 15(4), 217-221. Retrieved from https://www.imbiomed.com.mx/articulo.php?id=65272
- Giménez-Sánchez, F., Hernández-Borges, A., & Lara-Oya, A. (2016). Surfactant Therapy with INSURE Technique. Anales de Pediatría, 85(3), 144.e1-144.e7. DOI: 10.1016/j.anpedi.2015.11.015
- Integral Medical Assistance Program (PAMI). (2014). Administration of Exogenous Surfactant. Foundation for Maternal and Child Health (FUNDASAMIN). Retrieved from https://www.fundasamin.org.ar/web/wp-content/uploads/sites/10/2014/01/Administraci%C3%B3n-de-surfactante-ex%C3%B3geno.pdf





